Axial spondyloarthritis (axSpA) increases your likelihood of developing or experiencing other conditions. This is known as a co-morbidity. One of the co-morbidities that people with axSpA may experience is inflammatory bowel disease.
What is inflammatory bowel disease
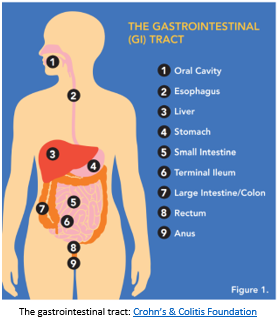 Inflammatory bowel disease, or IBD, is the term used to describe two different conditions, Crohn’s disease and ulcerative colitis. IBD occurs when the gastrointestinal tract, which runs from the mouth to the anus, becomes inflamed.
Inflammatory bowel disease, or IBD, is the term used to describe two different conditions, Crohn’s disease and ulcerative colitis. IBD occurs when the gastrointestinal tract, which runs from the mouth to the anus, becomes inflamed.
What are the symptoms?
The symptoms of IBD may include:
- Abdominal pain and/or cramping
- Diarrhoea
- Bloody stools
- Fatigue
- Low appetite
- Unintended weight loss
The symptoms you experience will depend on whether you have Crohn’s disease or ulcerative colitis and where in the gastrointestinal tract the disease is focussed.
What causes IBD in people with axSpA?
axSpA is what is known as an auto-immune disease. This means that the immune system becomes overactive and starts to attack healthy tissue, causing inflammation. In people with axSpA, this inflammation can occur in a number of different body systems, including the gastrointestinal tract, resulting in IBD.
People with axSpA are between 1 and 4 times more likely to develop IBD compared to the rest of the population.
How is IBD diagnosed?
If your rheumatologist, dermatologist or GP suspects you may have IBD, they will likely refer you to a gastroenterologist, a medical doctor who specialises in diseases of the gastrointestinal tract.
Aside from asking about your medical history, your doctor may also perform a physical examination or suggest a gastroscopy or a colonoscopy to help diagnose IBD. A number of different scans and blood tests may also be suggested to help rule out other conditions.
What will happen to me?
As with axSpA, your IBD symptoms can disappear and reappear over time. You will likely experience periods where your symptoms decrease or are inactive. This is known as being in ‘remission’. Periods where your symptoms are active are known as having a ‘flare’.
Once IBD has been diagnosed the condition can usually be effectively managed and most people with IBD lead full and productive lives. However, it is a chronic condition that may change over time and complications can occur that will require medical attention, particularly if the condition is not well-managed. Seeing your doctor regularly and keeping them informed when flares occur can help with this.
Can IBD be cured?
Unfortunately, IBD cannot be cured; however, with the right treatment, symptoms of IBD can be effectively managed and the impact of the disease and the likelihood of flares kept to a minimum.
What treatments are there for IBD?
Often treatments for IBD are similar to those recommended for axSpA Depending on whether your IBD is in remission or whether you are experiencing a flare you may find your doctor suggests one, or a combination, of the following:
- Corticosteroids. These will likely be used only for short periods to manage flares
- Immunomodulators. These medicines help to regulate the activity of the immune system to modify the disease process and reduce inflammation. They may be used for longer periods
- Biologic disease modifying anti-rheumatic drugs, often known as ‘biologics’ or ‘bDMARDs’. This newer class of medication modifies the disease process to reduce inflammation, but in a more targeted way. A number of different biologics are available and different ones work better for some people than others. Where possible, your gastroenterologist and rheumatologist should work together to find a bDMARD that will help both your IBD and your axSpA.
The use of non-steroidal anti-inflammatory drugs (NSAIDs), which also work to reduce inflammation, may make IBD symptoms worse, so their use in people with axSpA who experience IBD symptoms may not be recommended.
It may take some time to figure out the best treatment plan for you. Work with your doctor to figure out what works best for you in managing your axSpA and your IBD.
What can I do?
Aside from trying to ensure your axSpA is well-managed and seeing your doctor regularly, there is a lot you can do to help limit the impacts of IBD.
- While there are some foods that are more likely to aggravate IBD symptoms, such as fatty, greasy foods or sugary foods and drinks, everyone’s experience of IBD is different and there is little evidence that following a certain diet can help either your IBD or axSpA. Instead, it is important to find out what foods help you and what ones make your IBD symptoms worse. You may find keeping a food diary that tracks your symptoms can help you to figure out what works for you.
- Due to the loss of nutrients that comes with having IBD, it is important when figuring out what foods work for you that you also consider how to replace those lost nutrients. For example, if you find that eating raw vegetables makes your symptoms worse, try cooking them thoroughly so that you still get the nutritional benefits while minimising the impact on your IBD symptoms.
- Consider seeing a dietitian. These health professionals specialise in the impacts of diet on health and can help you figure out the balance between managing IBD symptoms and ensuring you get the nutrients you need to stay healthy.
- Consider taking a multi-vitamin or a mineral supplement. You should always discuss taking these with your doctor or dietitian to advise you whether this is necessary and which may be useful.
- Quit smoking. Smoking can make the symptoms of IBD worse and more difficult to treat.
- Speak to your doctor about ways to relieve discomfort from the symptoms of IBD, particularly if you are experiencing a flare.
- Speak with your GP about seeing a counsellor or psychologist if you feel you need to talk to someone about the impact IBD or axSpA is having on your mental wellbeing.
- Make sure you are looking to reliable sources for information on IBD and axSpA. A large amount of information is available online but not all of it is from reliable sources or based on scientific evidence. If you are unsure about the accuracy of any information, speak with your doctor.
For further information on IBD or to access support services see Crohn’s & Colitis Australia https://www.crohnsandcolitis.com.au/
This resources has been developed based on the best available evidence. A full list of references is available upon request.