Back pain is often one of the first symptoms of axial spondyloarthritis (axSpA) and is one of the main symptoms of managing axSpA. Living with pain can be one of the hardest parts of having arthritis. It is understandable that the ongoing physical symptoms such as chronic pain, fatigue and disturbed sleep can cause distress and affect your mood and your mental wellbeing. Understanding pain and learning techniques that may help you cope with pain are an important part of managing axSpA.
What is pain?
There are now thought to be three types of pain:
- Tissue damage or inflammation, the process that causes heat and swelling in your joints
- Nerve pain
- Increased sensitivity (hypersensitivity) of the pain system
For some conditions, such as fibromyalgia, the cause of the pain is not fully understood.
Pain signals may be triggered by:
- physical injury or damage to your body – for example, a sprained ankle or damage that occurs as part of a longer-term condition such as osteoarthritis.
- chemicals produced within the body itself that can irritate the nerve endings – this may be linked to an infection, an overuse injury or a flare-up of a long-term illness such as arthritis.
- damage to nerves that causes them to be more sensitive to pain signals and even non-painful stimuli that now can cause pain. This type of “nerve” pain is known as neuropathic pain.
- inflammation, the process that causes heat and swelling in your joints
- muscle tension, from trying to protect joints from painful movements
- Fibromyalgia, an autoimmune condition that can cause widespread pain and tenderness in the body.
What is long-term pain?
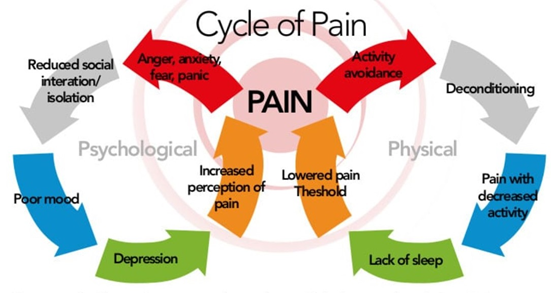
Doctors define long-term (or ‘chronic’) pain as pain that lasts for more than 3 months or pain that lasts for longer than would be expected for the type of injury or level of damage. For people living with axSpA ongoing pain is a real possibility and so it is important to not only relieve your pain, but also manage your underlying condition to minimise inflammation and damage to your joints. Because our bodies tend to understand pain as a warning sign, our natural reaction is often to protect the affected area from further harm – perhaps by resting it completely, by using it less than usual or by supporting it. After a time, this can lead to weakening of the muscles. As we become less fit, we tire more easily and become more prone to strains and sprains, resulting in further pain. This can easily become a vicious circle.
This is why, remaining active and getting help with a safe exercise program is an important part of managing your axSpA.
How can pain affect you?
The experience of pain is very personal. That is because pain does not occur in isolation but is influenced by many things such as stress, fatigue (tiredness) and your mood (anxiety and depression). For example, people who feel depressed or anxious have been found to be more sensitive to pain. This can make your pain feel worse, which can lead to a continuing cycle of fatigue and depression.
Other problems linked to long-term pain may include:
- sleep problems
- reduced physical activity
- difficulty with everyday activities
- reduced involvement in family and social activities
- difficulty concentrating or remembering things
- symptoms such as fatigue or weight gain
- side-effects from medications
- missing work, difficulties at work, or having to retire early
- changes in your relationships or sex life.
What can I do to manage my pain?
Pain may limit some of the things you do, but it doesn’t have to control your life. You can manage your pain by using some of the strategies described, below. What works for one person may not work for another, so you may have to try different techniques until you find what works best for you.
- Take medicines wisely. Most of the medicines used to treat pain from axSpA fall into one of the following categories:
Finding the right pain medications is about striking a balance between the benefits and the possible side-effects. These will vary from person to person and will also depend on how long they’re used for. A doctor or pharmacist can help you understand which medicines are right for you and how best to use them.
- Exercise. Research has shown that regular appropriate physical activity can help reduce pain. It also keeps your joints moving, strengthens muscles to support your joints, reduces stress and improves sleep. A health professional (e.g. a physiotherapist or exercise physiologist) or your doctor can help you work out a program suitable for you.
- Use heat and cold. The benefits of heat and cold for arthritis are yet to be proven by research. However, these treatments are soothing and safe when used carefully. Heat relaxes your muscles and stimulates blood circulation. You could try a warm bath or place a heat pack or hot water bottle over the painful area for 15 minutes. Cold numbs the painful area and reduces swelling. Applying cold treatments, such as ice packs, to the painful area for 15 minutes may be especially useful for hot, swollen joints, such as during a ‘flare’. You can repeat heat or cold treatments throughout the day. Make sure the temperature of your skin has returned to normal before re-applying, to prevent any tissue damage. Ask your doctor or physiotherapist whether heat or cold is best for you.
- Take care of your joints and save energy. Looking after your joints during your daily activities can help reduce pain, stress and tiredness. It involves simple habits such as: – avoiding activities that cause pain – asking for help when you need it – using special aids and gadgets to make tasks easier. Pace your activities so you can make the most out of your energy and get sufficient relaxation.
- Visit a pain management clinic. Pain management clinics can help you manage your pain with a range of different treatment options. Speak with your GP about whether you are eligible for a Chronic Disease Management Plan (CDMP). A CDMP will allow you to access allied health services required for ongoing treatment for your pain. Medicare rebates are available for certain services on referral from your GP.
- Mind techniques. A trained professional, such as a psychologist, can help you learn relaxation and pain coping skills so you can better manage your pain. Some of these techniques include:
- Cognitive behavioural therapy (CBT) is a form of talk therapy that helps people identify and develop skills to change negative thoughts and behaviours. By changing these negative thoughts and behaviours, you can change your awareness of pain and develop better coping skills, even if the actual level of pain stays the same.
- Relaxation: Relaxation techniques, such as deep breathing, guided imagery (mental pictures) and progressive muscle relaxation, can help you reduce stress and muscle tension. These techniques need to be practised and you may have to try several methods before you find one that works for you. You may find it helpful to use recordings, CDs, books, or mobile phone meditation apps to help you learn relaxation techniques.
- Mindfulness Based Stress Reduction (MBSR): This is a structured program developed by Professor Jon Kabat-Zinn at the University of Massachusetts Medical School, in the 1970s. MBSR helps you become aware of negative or exaggerated thoughts and how to respond to them to help break the cycle of anxiety, stress or depression. Programs are offered all around Australia. To find out more information speak with your health care provider.
- painTRAINER. painTRAINER is an interactive, online program based on scientific research that teaches you effective strategies to manage your pain.
- Massage. There are limited scientific studies that show massage may temporarily improve pain and mobility of joints and muscles. Make sure the massage therapist has experience working with people who have arthritis. You can find a qualified therapist by contacting the Australian Association of Massage Therapists, or the Institute of Registered Myotherapists of Australia.
- Acupuncture. Acupuncture is an ancient Chinese practice of putting small, thin needles into the skin at specific points on the body to block the pain signal. There is limited evidence about the effectiveness of acupuncture in arthritis. However, some people may find it useful alongside other proven treatments, such as medicines. The Australian Acupuncture and Chinese Medicine Association can help you find an accredited practitioner.
- Transcutaneous electrical nerve stimulation (TENS). A TENS machine applies very mild electric pulses to block pain messages going from the painful area to your brain. TENS can be useful for longer-term pain but does not work for all people. See a physiotherapist to trial a TENS machine, and to learn how to use it correctly, before you buy one.
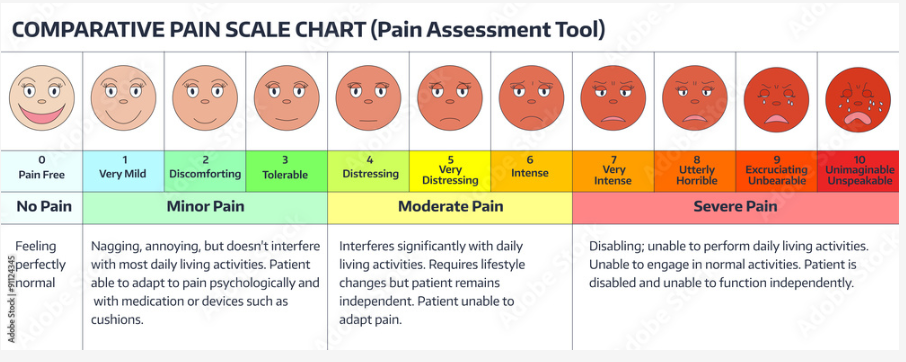
Pain scale chart
This pain scale chart can be used to rate your level of joint pain. Take it doctor's appointment to discuss your level of pain with your doctor.
Useful links
- https://www.painaustralia.org.au/ - find information resources on pain and support services.
- https://www.painrevolution.org/
Contact your local Arthritis Office for details of self-management courses that can teach you pain management techniques.
You may also find the Arthritis Australia information booklet helpful. Taking control of Your Pain in Arthritis