Already pregnant or just starting to think about pregnancy? Becoming a parent is one of the most exciting and overwhelming times in most people’s lives. But even more so if you, or your partner, has axial spondyloarthritis (axSpA).
I have axSpA…is having a family possible?
Absolutely. It might require extra planning and patience, or not be quite as you pictured it, but becoming a parent is usually possible if you have axSpA.
The journey to parenthood can be uncertain and demanding, often both physically and emotionally, and sometimes more so if you are living with axSpA. Living with joint pain and other symptoms can make it challenging to care for a new baby or an active toddler. However, with proper planning and medical care, most people with axSpA can have safe, successful pregnancies and become loving, capable parents.
The first step on the path towards parenthood is to discuss your family plans with your rheumatology team before you start trying for a baby
Does having axSpA make it harder to fall pregnant?
Evidence suggests that if you or your partner have inflammatory arthritis, like axSpA it may take longer to conceive. Experts aren’t sure why this is the case. It could be due to the disease itself or some arthritis medications, such as anti-inflammatory medications. Other factors such as lower sex drive due to fatigue and pain might also play a role.
It is estimated that as many as one in six couples in the Australian population have trouble conceiving, so if this is an issue for you, you are definitely not alone. The good news is that advances in medicine and science have made treatments for fertility more effective.
If you have any concerns about your fertility, speak to your GP or rheumatologist who can refer you to a fertility specialist, such as an obstetrician, to improve your chances of getting pregnant. It can be a lonely, emotionally draining experience if it’s taking longer than you had hoped to fall pregnant, especially if you have ceased some of your medications in order to conceive safely.
Is there an increased risk of miscarriage or problems during pregnancy if I have axSpA?
Most studies have found that the rates of miscarriage for women with axSpA are no different from rates for women without axSpA .
There is also no increased risk of miscarriage if the father has axSpA . Most types of axSpA that are well controlled don’t increase the risk of complications during pregnancy or cause harm to the unborn baby.
Highly active, or poorly controlled axSpA can cause risks for both you and your unborn baby, so it is vital to work with your healthcare team to find a management plan that works for you.
Can axSpA be passed on to my unborn baby?
If you or your partner carry the HLA-B27 gene there is a chance your child could inherit the gene. But this does not mean they will necessarily develop axSpA.
If you are worried, it’s a good idea to talk to your rheumatologist for more specific information.
We want to start a family – what do I need to consider?
Get the right advice – see your rheumatologist before planning for a baby. Some of the medications used to treat axSpA can be taken safely before and throughout pregnancy. Some can be used at certain times during pregnancy. Others are harmful to a growing baby so shouldn’t be used during pregnancy. Some medications remain in your body for many months after you stop taking them so you may need to wait a while before trying to conceive.
If you or your partner has axSpA , make it a priority to talk to your rheumatologist at least six months before you start trying to conceive.
Your rheumatologist can give you advice about the safest combination of medicines to continue taking during conception and pregnancy, other treatments you could use while trying to conceive, and which medicines should be stopped before conception (and when you should stop them).
Suddenly stopping your medications could make your axSpA worse, which can cause health problems for both you and your baby. Always talk to your rheumatologist before you stop taking any of your arthritis medications. Remember, there are many arthritis medications that can be safely used before and during pregnancy.
Questions for your healthcare team
Here are some things to discuss with your healthcare team, such as your rheumatologist, rheumatology nurse and GP before you start trying to conceive:
1. Are there any medications in my treatment plan that I should stop taking while I’m trying to fall pregnant or when I am pregnant? If yes:
- How long should I stop taking the medication(s) before I start trying for a baby?
- What are my other options to help manage my symptoms while I can’t take my usual medication?
2. Are there any medications for axSpA that are safe to continue while I’m trying for a baby, and during pregnancy?
3. Do I need any vaccinations before trying for a baby, or if my medications are changing?
4. Should I be taking any supplements before trying to fall pregnant?
5. When would be the best time for my partner and I to start trying for a baby?
6. What is the best type of contraception we should be using while we’re waiting to conceive?
7. Are there any tests I need before trying to conceive?
Your medical team should be able to work with you to come up with a treatment plan that protects the health of your unborn baby, while also keeping your axSpA under control. Be mindful that treatment plans may need to change, or you may need to try a range of different medications to find the right treatment for you during this period.
If you find it hard to talk openly and honestly with your doctor about your options or concerns, write down your questions before the appointment. You can also consider seeking a second opinion from another rheumatologist with a special interest in pregnancy.
Does it matter how active my axSpA is before I conceive?
You might be eager to start a family, but your rheumatologist only wants to talk about how to get your axSpA under better control. Why does it matter whether your axSpA is active if you’re trying to conceive? Conceiving while your arthritis is not well controlled or highly active can cause risks for both you and your unborn baby.
Having your axSpA well controlled may:
- make it easier for you to conceive
- reduce your chance of requiring a caesarean section to deliver your baby
- reduce the chance of your baby being born prematurely, or having a low birth weight
- prevent permanent joint damage and disability to you.
It is vital to work with your rheumatology team to find a plan that works for you and puts you on the path to a healthy pregnancy and baby.
What about men with axSpA ?
If you are a man with axSpA and you are thinking about starting a family, your medications could also affect your fertility or your unborn baby. Most medications can still be taken but some may need to be stopped, possibly for several months, before trying for a baby. Some medications can reduce your sperm count, although this is usually reversed when you stop taking them.
Talk to your rheumatologist at least six months before you and your partner plan to conceive.
Your rheumatologist can give you advice about the best treatment plan to follow before conceiving. Be vigilant with contraception to prevent unplanned pregnancies until you are ready to conceive.
When is the best time to start trying for a baby?
The best time to start trying for a baby is when your axSpA is well controlled or stable. While you might get a sense of this yourself from monitoring your own symptoms, it is important you discuss with your rheumatologist whether your axSpA is stable.
If your axSpA is not well controlled, you may find it harder to conceive and there can be risks for both you and your unborn baby. Talk to your rheumatologist about the best management plan that will give you the best chance of achieving your goal of becoming a parent while also protecting the health of you and your baby.
You may also need to wait after stopping certain medications; for example, methotrexate needs to be stopped at least three months before trying to conceive.
Stop smoking and avoid recreational drugs to reduce the risk of harm to your baby. Eat a healthy balanced diet, lose any extra body weight, start taking a folic acid supplement and lead a healthy lifestyle to further boost your chances of a healthy pregnancy.
What is the current evidence about medication safety for pregnancy and breastfeeding?
If you are planning a pregnancy it is vital to get an expert opinion from your rheumatologist about your medications as early as possible. Some arthritis medications are safe to continue before and during pregnancy. Other medications may need to be stopped as they may increase the risk of miscarriage or cause harm to a developing baby. Your rheumatologist will work with you to find the right arthritis management plan for both your health and the health of your unborn baby.
The current evidence about the safety of medications is summarised on the below table. This is a general guide only. New information is being discovered regularly and advice may be updated. Use this table to discuss your medications with your rheumatologist and always follow their expert advice.
Unplanned pregnancy
If you, or your partner, have fallen pregnant unexpectedly, call your rheumatologist or treating doctor immediately.
If you are taking any of the medications from the "Not safe" column in the table below, stop taking them as soon as you find out you are pregnant and contact your doctors.
If you are taking any of the medications from the "Generally safe" or "May be safe" columns in the table below, continue taking them as usual until you speak to your rheumatologist. Do not stop taking these medications without first talking to your rheumatologist and getting the right advice.
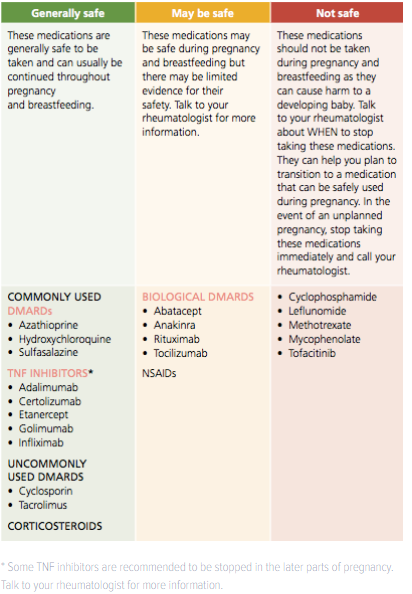
Pregnancy and axSpA – what can I expect when expecting* Some TNF inhibitors are recommended to be stopped in the later parts of pregnancy. Talk to your rheumatologist for more information.
The day you’d been hoping for has arrived…you’ve had a positive pregnancy test and you are now taking your first steps towards parenthood. Congratulations!
How will I feel during pregnancy?
The greatest myth of pregnancy… the pregnancy glow!
How your body will respond to pregnancy, and how you will feel during the next nine months, will be different for everyone. Every woman is unique, and every woman’s pregnancy is also unique.
Some women sail through pregnancy and even find that that their axSpA symptoms go into remission (their symptoms improve or completely disappear) during pregnancy. But that does not happen for every mother-to-be.
However, the pregnancy ‘glow’ that fills our newsfeed is a myth for many women, even without arthritis. Pregnancy can bring with it many unpleasant symptoms, which can be even more challenging if you have arthritis.
Pregnancy and axSpA remission
During pregnancy, your immune system goes through some changes to allow your baby to grow and develop.
For some women with axSpA, these changes to the immune system also bring a benefit of reducing the activity of their axSpA. It is thought that about half of women with axSpA will find that their symptoms, such as pain, stiffness and flares, improve during pregnancy.
However, there are many women with axSpA who continue to have active disease during their pregnancy. You may even find that your symptoms worsen, or you have disease flares, particularly if you’ve had to stop or change medications.
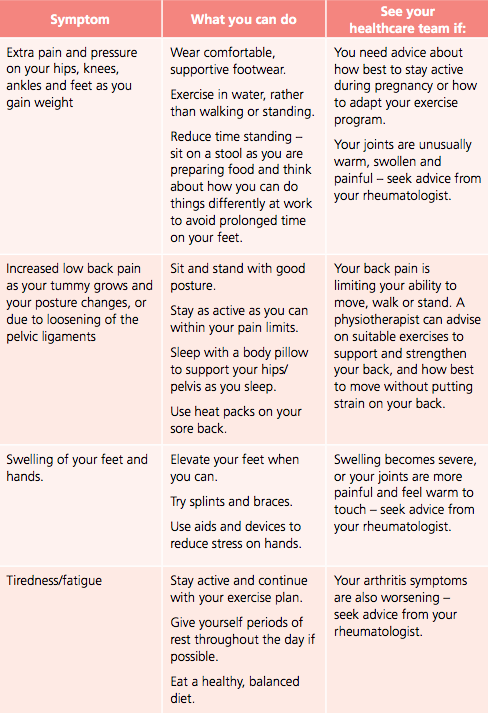
Physical effects of pregnancy
Pregnancy brings with it many physical changes to your body. If you are living with axSpA, some of these changes may even make your axSpA symptoms feel worse. Here are some common symptoms in pregnancy and tips for managing them:
Emotional health during pregnancy
Pregnancy can have a powerful effect on your mood, thoughts and emotions. Changes in your hormone levels can leave you feeling like you’re on an emotional rollercoaster at times, not to mention the impact of possible morning sickness, physical changes and bone-crushing tiredness. Some emotional ‘ups and downs’ are a normal part of pregnancy. However, if are feeling constantly sad, worried, scared or nervous, thinking negative thoughts about yourself, or are finding it difficult to sleep, eat or do the usual activities in your life, seek support.
Changes in your hormone levels can leave you feeling like you’re on an emotional rollercoaster at times
Talk to your GP or obstetrician about how you’re feeling, and they can suggest the best treatment options. You can also call the Perinatal Anxiety & Depression Australia (PANDA) National Helpline on 1300 726 306 for advice.
Labour and delivery
Throughout your pregnancy, you will no doubt hear many birth stories – some good, some bad and others you would rather not have heard! As these stories reveal, each birth is unique and rarely are they perfectly what the parents imagined.
Towards the end of your pregnancy, talk to your rheumatologist or obstetrician and/or midwife about how your axSpA could potentially impact on your delivery, such as:
- The positions you could use during labour and delivery. For example, there might be some positions that might be more comfortable if you have difficulties with your hips or lower back.
- Your ability to deliver your baby vaginally.
- If you have genital psoriasis that could impact the sensitivity of your skin.
- The likelihood of requiring a caesarean section. Remember, while a caesarean section is more common in women with arthritis, many women without arthritis are also advised not to deliver their babies vaginally. A caesarean section may be the best option for a healthy baby.
- Your ability to have an epidural or spinal anaesthetic (pain relieving medications into the spine) during labour, especially if you have arthritis that affects your spine.
It is easy to get overwhelmed by the pressure to have a ‘normal’ vaginal birth. However, the most important goal at the end of your pregnancy is for both you and your baby to be healthy. Try not to get too preoccupied by the idea of a perfect birth. Instead, surround yourself with healthcare professionals who you trust, and keep your focus on that all-important end goal, a healthy, happy baby and mum.
Talk to your healthcare team about how your axSpA could potentially impact on your baby’s delivery.
Life with a new baby
The arrival of your tiny bundle of joy will undoubtedly change your life forever. Caring for a new baby is equal parts exciting and exhausting for all new parents. And, as a parent with axSpA, you may even experience some additional challenges.
Find out more with our life with a new baby resource.
Seeking support
Who can help?
Rheumatologists are doctors who specialise in diseases of the joints. Your doctor will need to refer you to a rheumatologist. They may recommend a rheumatologist, or you can contact the Australian Rheumatology Association to find a rheumatologist.
A rheumatology nurse, if available, can help you understand your treatments, provide support and refer you to other health professionals.
A physiotherapist (physio) can use various treatments to keep your joints as flexible, strong and pain-free as possible. They will also show you exercises and pain-relief techniques to use at home.
An occupational therapist (OT) can provide advice on how to care for your baby without putting strain on your joints, including suggesting equipment and aids that can help.
Talk to your GP if you are finding your feelings and emotions are getting in the way of enjoying your life. They can suggest ways to cope, recommend medications that can help or refer you to a psychologist who can help you work through your feelings. You may be eligible for a Mental Health Care Plan, via your GP, which will provide subsidised sessions. You can also see a psychologist without needing a referral.
Perinatal Anxiety and Depression Australia (PANDA) supports women, men and families across Australia affected by anxiety and depression during pregnancy and early parenthood.
beyondblue provides information and advice about depression, anxiety, available treatments and where to get help.
Child health nurses are a wealth of information and support as you learn to care for your new baby. Ask your obstetrician or midwife or contact your local community health centre to find out about services in your area.
Lactation consultants can help you with any problems you might have with breastfeeding. Find out if your local hospital or child health clinic provides this service, otherwise you can pay for a private consultation.
The Australian Breastfeeding Association has a helpline 1800 mum 2 mum (686 268) and online forum to help you with any breastfeeding concerns.
The Independent Living Centre has information about aids and devices that can help with day-to-day activities.
Useful resources
The web can be a useful source of information and support. However, not everyone who puts information on the web is a qualified health practitioner. Some organisations make unrealistic promises in order to sell their products. Treatment options and practices from overseas may also not be relevant or approved in Australia. Always check information from the web with a trusted member of your healthcare team.
The Australian Government’s HealthDirect is an excellent starting point for web searches, as every site that HealthDirect links to has been checked for quality and accuracy of information.
Australian resources
Arthritis Australia’s website for people living with inflammatory arthritis www.empowered.org.au has a detailed section on pregnancy, including hearing directly from women with arthritis about their journeys to motherhood.
The Australian Rheumatology Association has a detailed document that outlines the most current evidence about the safety of arthritis medications during pregnancy.